There are a number of ways you can reduce your chances of experiencing migraines.
Identifying and avoiding triggers
One of the best ways of preventing migraines is recognising the things that trigger an attack and trying to avoid them.

2 days ago Migraine headaches cause a painful throbbing or intense pulsating usually in one side or area of the head. Migraine headaches can last anywhere from 4 to 72 hours and are recurring. The Prevention and Treatment Of Headaches (PLR) Private Label Rights Private Label Rights is a product that offers one of the best licenses around. PLR gives the user the rights to do just about anything they are wanting to do with it. The Prevention and Treatment Of Headaches (PLR) Private Label Rights Private Label Rights is a product that offers one of the best licenses around. PLR gives the user the rights to do just about anything they. Headache is a common problem that causes a lot of disturbance in life. Headache is usually a pain that occurs in any part of the head. Factors of Headache: There can be many factors that cause headaches: ⦁ Emotional (stress, anxiety, and depression) ⦁ Medical issue (migraine, high blood pressure, physical injury) Types of Headache.
You may find you tend to have a migraine after eating certain foods or when you're stressed, and by avoiding this trigger you can prevent a migraine.
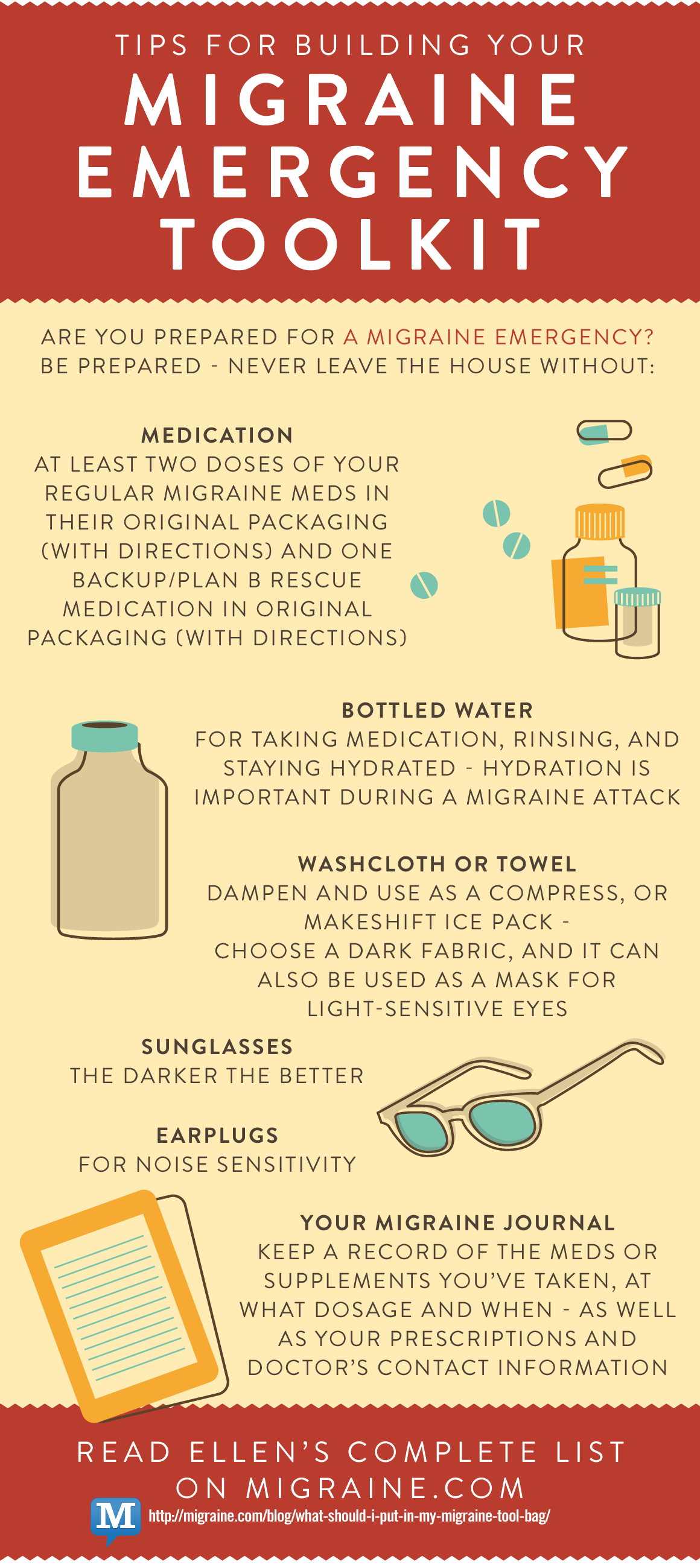
Keeping a migraine diary can help you identify possible triggers and monitor how well any medicine you're taking is working.
In your migraine diary, try to record:
- the date of the attack
- the time of day the attack began
- any warning signs
- your symptoms (including the presence or absence of aura)
- what medicine you took
- when the attack ended
Medicines and supplements
Medicines are also available to help prevent migraines. These medicines are usually used if you have tried avoiding possible triggers but you're still experiencing migraines.
You may also be prescribed these medicines if you experience very severe migraine attacks, or if your attacks happen frequently.
Some of the main medicines used to prevent migraines are outlined below.
Topiramate
Topiramate is a type of medicines originally developed to prevent seizures in people with epilepsy, but is now much more commonly used in migraine.
It's been shown to help prevent migraines, and is usually taken every day in tablet form.
Topiramate should be used with caution in people with kidney or liver problems.
It can also harm an unborn baby if taken during pregnancy and can reduce the effectiveness of hormonal contraceptives.
GPs should discuss alternative methods of contraception for women who are prescribed topiramate.
Side effects of topiramate can include:
- decreased appetite
- feeling sick
- being sick
- constipation or diarrhoea
- drowsiness
- problems sleeping
Propranolol
Propranolol is a medicine traditionally used to treat angina and high blood pressure, but it's also been shown to effectively prevent migraines.
It's usually taken every day in tablet form.
Propranolol is not suitable for people with asthma, chronic obstructive pulmonary disease (COPD) and some heart problems.
It should be used with caution in people who have diabetes.
Side effects of propranolol can include:
- cold hands and feet
- problems sleeping
- tiredness
Amitriptyline
Amitriptyline is a medicine originally designed to treat depression, but has also proved useful in helping prevent migraines.
It's usually taken every day in tablet form.
Amitriptyline can make you feel sleepy, so it's best to take it in the evening or before you go to bed.
Other side effects include:
- constipation
- dizziness
- a dry mouth
- difficulty peeing
- a headache
It may take up to 6 weeks before you begin to feel the full benefit of the medicine.
Botulinum toxin type A
In June 2012, NICE recommended the use of a medicine called botulinum toxin type A by headache specialists to prevent headaches in some adults with long-term migraine.
Best Treatment For Cluster Headaches
Botulinum toxin type A is a type of nerve toxin that paralyses muscles.
It's not exactly clear why this treatment can be effective for migraine.
NICE recommends that this treatment can be considered as an option for people who have chronic migraine (headaches on at least 15 days of every month, at least 8 days of which are migraine) that's not responded to at least 3 previous preventative medical treatments.
Under the NICE guidelines, botulinum toxin type A should be given by injection to between 31 and 39 sites around the head and back of the neck.
A new course of treatment can be given every 12 weeks.
Acupuncture
If medicines are unsuitable or do not help prevent migraines, you may want to consider acupuncture.
NICE states that a course of up to 10 sessions over a 5- to 8-week period may be beneficial.
Preventing menstrual-related migraines
Menstrual-related migraines usually occur from 2 days before the start of your period to 3 days after.
As these migraines are relatively predictable, it may be possible to prevent them using either non-hormonal or hormonal treatments.
Non-hormonal treatments
The non-hormonal treatments that are recommended are:
- non-steroidal anti-inflammatory drugs (NSAIDs) – a common type of painkiller
- triptans – medicines that reverse the widening of blood vessels, which is thought to be a contributory factor in migraines
These medicines are taken as tablets 2 to 4 times a day from either the start of your period or 2 days before, until the last day of bleeding.
Hormonal treatments
Hormonal treatments that may be recommended include:
- combined hormonal contraceptives, such as the combined contraceptive pill, patch or vaginal ring
- progesterone-only contraceptives, such as progesterone-only pills, implants or injections
- oestrogen patches or gels, which can be used from 3 days before the start of your period and continued for 7 days
Hormonal contraceptives are not usually used to prevent menstrual-related migraines in women who experience aura symptoms because this can increase your risk of having a stroke.
Read about the complications of migraines for more information about this.
Advice and support
There are a number of organisations that offer advice and support for people with migraines, including The Migraine Trust.
The Migraine Trust can be contacted on 020 7631 6970 or by emailing info@migrainetrust.org.
You can also join The Migraine Trust's online community through Facebook.
Video: migraine
This video explains how identifying and avoiding things that trigger migraines is an important part of managing them.
Media review due: 1 July 2023
Page last reviewed: 10 May 2019
Next review due: 10 May 2022
Allergy Headache
Symptoms: Generalized headache; nasal congestion; watery eyes
Precipitating Factors: Seasonal allergens, such as pollen, molds. Allergies to food are not usually a factor.
Treatment: Antihistamine medication; topical, nasal cortisone-related sprays; or desensitization injections
Prevention: None
Learn more about the relationship between allergies and headaches.
Aneurysm
Symptoms: May mimic frequent migraine or cluster headaches, caused by balloon-like weakness or bulge in the blood vessel wall. May rupture (stroke) or allow blood to leak slowly resulting in a sudden, unbearable headache, double vision, rigid neck. The individual rapidly becomes unconscious.

Precipitating Factors: Congenital tendency; extreme hypertension
Treatment: If an aneurysm is discovered early, treat with surgery.
Prevention: Keep blood pressure under control.
Arthritis Headache
Symptoms: Pain at the back of the head or neck which intensifies on movement. It is caused by inflammation of the blood vessels of the head or bony changes in the structures of the neck.
Precipitating Factors: The cause of pain is unknown
Treatment: Anti-inflammatory drugs, muscle relaxants
Prevention: None
Caffeine-Withdrawal Headache
Symptoms: Throbbing headache caused by rebound dilation of the blood vessels, occurring multiple days after consumption of large quantities of caffeine.
Precipitating Factors: Caffeine
Treatment: Treat by terminating caffeine consumption in extreme cases.
Prevention: Avoiding excess use of caffeine.
The NHF project “New Perspectives on Caffeine and Headache” has all the information you need about the complex relationship between headache and caffeine.
Cervicogenic Headache
Symptoms: Pain on one side of the head or face, stiff neck, pain around the eyes, neck, shoulder, and arms, nausea, blurred vision, sensitivity to light and sound.
Precipitating Factors: Injury to the neck, malformations of the cervical vertebrae, arthritis of the upper spine
Treatment: Treatment varies depending on the severity of symptoms, non-steroidal anti-inflammatories (aspirin or ibuprofen), nerve blocks, physical therapy, transcutaneous electrical nerve stimulation (TENS), neuromodulation surgery
Prevention: Without treatment, a cervicogenic headache can become debilitating.
Chronic Daily Headache
Symptoms: Refers to a broad range of headache disorders occurring more than 15 days a month; two categories are determined by the duration of the headache (less than four hours and more than four hours).
Precipitating Factors: Typically evolve from transformed migraine. Although not related to chronic tension-type headache, they can evolve from episodic tension-type headache. Can be associated with medication overuse.
Treatment: Depending on the type of CDH, different treatment options exist. It is important to limit analgesic use.
Prevention: Based on the diagnosis of headache, how long they last, and the number experienced per month.

Chronic Migraine
Symptoms: Headache occurring more than 15 days a month, for more than 3 months, which has the features of migraine headache on at least 8 days per month.
Precipitating Factors: Often associated with Medication Overuse Headache (MOH) or Rebound Headache. Can occur without MOH and be associated with major life events, obesity, ineffective acute medications.
Treatment: After drug withdrawal, headaches will either revert to episodic or remain chronic. Botox and CGRP monoclonal antibodies have been approved for use in chronic migrane.
Cluster Headache
Symptoms: Excruciating pain in the vicinity of the eye; tearing of the eye; nose congestion; and flushing of the face. Pain frequently develops during sleep and may last for several hours. Attacks occur every day for weeks, or even months, then disappears for up to a year. Eighty percent of cluster patients are male, most between the ages of 20 and 50.
Precipitating Factors: Alcoholic beverages; excessive smoking
Treatment: Oxygen; ergotamine; sumatriptan; or intranasal application of local anesthetic agent
Prevention: Use of steroids; ergotamine; calcium channel blockers; and lithium
Depression and Headache
Symptoms: People with painful diseases tend to become depressed.
Precipitating Factors: Causes can originate from a wide variety of complaints that can be categorized as physical, emotional, and psychic.
Treatment: The presence of depression is often subtle and the diagnosis is frequently missed. Depression is a widespread affliction that can be treated, but first, it must be unmasked.
Prevention: Physicians can prescribe tricyclic antidepressants, selective serotonin reuptake inhibitors, or monoamine oxidize inhibitors in the treatment of headaches associated with depression.
Eyestrain Headache
Symptoms: Usually frontal, bilateral pain directly related to eyestrain. It is a rare cause of headache.
Precipitating Factors: Muscle imbalance; uncorrected vision; astigmatism
Treatment: Correction of vision
Prevention: Correction of vision
Exertional Headache
Symptoms: Generalized head pain of short duration (minutes to an hour) during or following physical exertion (running, jumping, or sexual intercourse), or passive exertion (sneezing, coughing, moving one’s bowels, etc.)
Precipitating Factors: Ten percent caused by organic diseases (aneurysms, tumors, or blood vessel malformation). Ninety percent are related to migraine or cluster headaches.
Treatment: Cause must be accurately determined. Most commonly treated with indomethacin or propranolol. Extensive testing is necessary to determine the headache cause. Surgery is occasionally indicated to correct the organic disease.
Prevention: Alternative forms of exercise; avoid jarring exercises
Fasting Headache
Symptoms: Frontal location, with diffuse, non-pulsating pain of milt-to-moderate intensity.
Precipitating Factors: Caused by fasting
Treatment: Headache should resolve in less than 72 hours after eating
Prevention: Eat multiple small meals daily
Fever Headache
Symptoms: Generalized head pain that develops with fever and is caused by the swelling of the blood vessels of the head.
Precipitating Factors: Caused by infection
Treatment: Aspirin; acetaminophen; NSAIDs; antibiotics
Prevention: None
Giant Cell Arteritis
Symptoms: A boring, burning, or jabbing pain caused by inflammation of the temporal arteries; pain, often around the ear, when chewing; weight loss; eyesight problems. This rarely affects people under 50.
Precipitating Factors: Maybe due to vascular disease characterized by inflammation of the blood vessels.
Treatment: Treat with oral corticosteroids after diagnosis; confirmed by biopsy of the temporal artery. Detected by erythrocyte sedimentation rate (ESR) and C-reactive protein test.
Prevention: None
Hangover Headache
Symptoms: Migraine-like symptoms of throbbing pain and nausea, but it is not localized to one side.
Precipitating Factors: Alcohol, which causes dilation and irritation of the blood vessels of the brain and surrounding tissue.
Treatment: Liquids (including broth); consumption of fructose (honey, tomato juice are a good source)
Prevention: Drink alcohol only in moderation
Headache Attributed to Infection
Symptoms: Diffuse, moderate-to-severe pain caused by acute infection, accompanied by fever.
Precipitating Factors: Infections
Treatment: Aspirin, acetaminophen, NSAIDs, antibiotics as needed.
Prevention: No
Hemiplegic Migraine
Symptoms: Stroke-like symptoms- Severe throbbing pain, often on one side of the head, numbness, weakness or paralysis on one side of the body, nausea, vomiting, dizziness, loss of balance, speech difficulties, visual disturbances, auras, sensitivity to light, sound, and smell.
Precipitating Factors: Hemiplegic migraine has a strong genetic component
Treatment: Once confirmed, treatment should consist of dietary modification to avoid triggers, regular exercise and sleep, and dietary supplementation, such as magnesium. Topiramate, valproic acid, and calcium channel blockers have shown the best pharmacologic results. Triptans must be avoided to prevent severe complications. Such care is best provided under the supervision of a multidisciplinary headache clinic or a specialized neurologist.
Prevention: Preventive medications, dietary modification to avoid triggers, regular exercise and sleep
Hunger Headache
Symptoms: Pain strikes just before mealtime. It is caused by muscle tension, low blood sugar, and rebound dilation of the blood vessels, oversleeping, or missing a meal.
Precipitating Factors: Strenuous dieting or skipping meals
Treatment: Regular, nourishing meals containing adequate protein and complex carbohydrates
Prevention: Regular, nourishing meals containing adequate protein and complex carbohydrates
Hypertension Headache
Symptoms: Generalized or “hairband” type of pain that is most severe in the morning. It diminishes throughout the day.
Precipitating Factors: Severe hypertension: over 200 systolic and 110 diastolic
Treatment: Treat with appropriate blood pressure medication
Prevention: Keep blood pressure under control
One member asks George Nissan, DO about the relationship between hypertension and headaches. Read Dr. Nissan’s answer here.
Menstrual Headache
Symptoms: Migraine-type pain that occurs shortly before, during, or immediately after menstruation or at mid-cycle (at time of ovulation).
Precipitating Factors: Variances in estrogen levels
Treatment: At the earliest onset of symptoms, treat using biofeedback, ergotamine, dihydroergotamine, or a 5-HT agonist. Once the pain has begun, treatment is identical to migraine without aura.
Prevention: Biofeedback; beta-blockers (propranolol, timolol); anti-convulsant (divalproex sodium); calcium blockers; and NSAIDs
Migraine with Aura
Symptoms: Warning signs develop, which may include visual disturbances or numbness in the arm or leg. Warning symptoms subside within 30 minutes followed by severe pain.
Precipitating Factors: There is a hereditary component. Other factors include certain foods; the Pill or menopausal hormones; excessive hunger; changes in altitude; weather; lights; excessive smoking; and emotional stress.
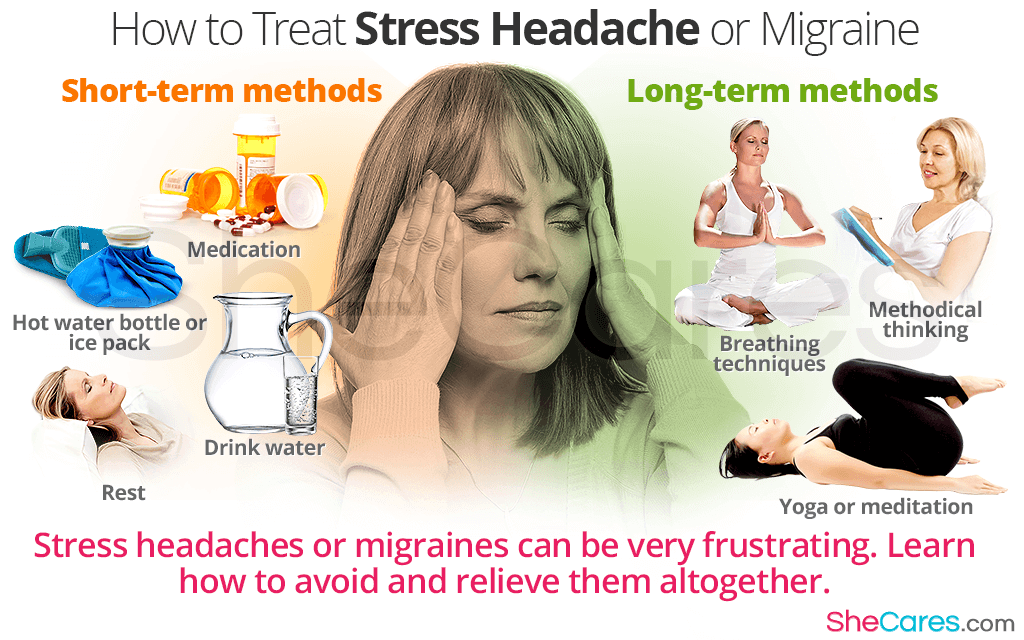
Treatment: At the earliest onset of symptoms, treat using biofeedback, ergotamine, dihydroergotamine, or a 5-HT agonist. Once the pain has begun, treat with: ice packs; isometheptene; mucate; combination products containing caffeine; ergotamine; DHE injectable and nasal spray; 5-HT agonists; analgesics or medications, which constrict the blood vessels. Steroids may be helpful for prolonged attacks.
Prevention: Biofeedback; beta-blockers (propranolol, timolol); anti-convulsant (divalproex sodium); calcium blockers; and NSAIDs. CGRP monoclonal antibodies were recently approved for prevention.
Migraine without Aura
Symptoms: Severe, one-sided throbbing pain, often accompanied by nausea, vomiting, cold hands, sensitivity to sound and light
Precipitating Factors: There is a hereditary component. Other factors include certain foods; the Pill or menopausal hormones; excessive hunger; changes in altitude; weather; lights; excessive smoking; and emotional stress.
Treatment: Ice packs; isometheptene; mucate; combination products containing caffeine; ergotamine; DHE injectable and nasal spray; 5-HT agonists; analgesics or medications, which constrict the blood vessels. Steroids may be helpful for prolonged attacks. CGRP monoclonal antibodies were recently approved for prevention.
Prevention: Biofeedback; beta-blockers (propranolol, timolol); anti-convulsant (divalproex sodium); calcium blockers; and NSAIDs
New Daily Persistent Headache
Symptoms: Best described as the rapid development (less than three days) of unrelenting headache. Typically presents in a person with no past history of headache.
Precipitating Factors: Does not evolve from migraine or episodic tension-type headache. It begins as a new headache and may be the result of a viral infection.
Treatment: Can resolve on its own within several months. Other cases persist and are more refractory.
Prevention: Does not respond to traditional options, but anti-seizure medications, Topamax, or Neurontine can be used.
Post-Traumatic Headaches
New Cluster Headache Treatment
Symptoms: Localized or generalized pain, can mimic migraine or tension-type headache symptoms. Headaches usually occur on a daily basis and are frequently resistant to treatment.
Precipitating Factors: Pain can occur after relatively minor traumas, but the cause of the pain often difficult to diagnose.
Treatment: Possible treatment by the use of anti-inflammatory drugs, propranolol, or biofeedback
Prevention: Standard precautions against trauma
Sinus Headache
Symptoms: Gnawing pain over the nasal area, often increasing in severity throughout the day. Pain is caused by acute infection, usually with fever, producing blockage of sinus ducts, and preventing normal drainage. Sinus headaches are rare. Migraine and cluster headaches are often misdiagnosed as sinus in origin.
Precipitating Factors: Infection, nasal polyps, anatomical deformities, such as deviated septum that blocks the sinus ducts
Treatment: Treat with antibiotics, decongestants, surgical drainage, if necessary
Prevention: None
Temporomandibular Joint (TMJ) Headache
Symptoms: A muscle-contraction type of pain, sometimes accompanied by a painful “clicking” sound on the opening of the jaw. It is an infrequent cause of headache.
Precipitating Factors: Caused by malocclusion (poor bite), stress, and jaw clenching
Treatment: Relaxation, biofeedback, and the use of a bite plate are the most common treatments. In extreme cases, the correction of malocclusion may be necessary
Prevention: Same as treatment
Tension-Type Headache
Symptoms: Dull, non-throbbing pain, frequently bilateral, associated with tightness of scalp or neck. The degree of severity remains constant.
Precipitating Factors: Emotional stress, hidden depression
Treatment: Rest; aspirin; acetaminophen; ibuprofen; naproxen sodium; combinations of analgesics with caffeine; ice packs; muscle relaxants; antidepressants, if appropriate; biofeedback; psychotherapy; temporary use of stronger prescription analgesics, if necessary.
Tension Headache Prevention
Prevention: Avoidance of stress; use of biofeedback; relaxation techniques; or antidepressant medication
Tic Douloureux Headache (Trigeminal Neuralgia)
Symptoms: Short, jab like pain in trigger areas found in the face around the mouth or jaw; frequency and longevity of pain varies. It is a relatively rare disease of the neural impulses and is more common in women after age 55.
Precipitating Factors: Cause unknown, pain from chewing, cold air, touching the face. If under age 55, may result from neurological diseases, such as MS.
Treatment: Anticonvulsants and muscle relaxants, neurosurgery
Prevention: None
Thunderclap Headache
Symptoms: Sudden and severe pain that may be accompanied by nausea, vomiting, fever, seizure speech problems, weakness, confusion, visual disturbances.
Precipitating Factors: Thunderclap Headache may be due to a benign syndrome or a potentially life-threatening condition.
Treatment: Since the nature of the headache by itself cannot allow the distinction between benign and serious causes, it is essential to seek out an emergency medical evaluation if the onset of a headache is sudden and severe.
Prevention: None
Tumor Headache
Symptoms: Pain progressively worsens; projectile vomiting; possible visual disturbances speech or personality changes; problems with equilibrium; gait, or coordination; seizures. It is an extremely rare condition.
Migraine Headache Prevention
Precipitating Factors: The cause of the tumor is usually unknown.
Treatment: If discovered early, treat with surgery or newer radiological methods.
Headache Prevention Medications
Prevention: None
